チェア コーデ 5本脚 ハイバック K04-PF31SC-T7T71 66911647 送料無料 コクヨ kokuyo
(税込) 送料込み
商品の説明
商品情報
●商品名 チェア コーデ 5本脚 ハイバック ●コクヨ品番 K04-PF31SC-T7T71 ●メーカー コクヨ KOKUYO ●サイズ 幅680mm 奥行550mm 高さ850mm ●重量12kg ●代引き不可商品
53979円チェア コーデ 5本脚 ハイバック K04-PF31SC-T7T71 66911647 送料無料 コクヨ kokuyo家具、インテリアオフィス家具楽天市場】コクヨ ミーティングチェア 会議イス CORne コルネ K07-DZ72"https://item-shopping.c.yimg.jp/i/j/kokuyofn_fn102394","https://item-shopping.c.yimg.jp/i/j/kokuyofn_fn102392","https://tshop.r10s.jp/kokuyofn/cabinet/coode/fn102419.jpg","https://image1.shopserve.jp/e-aocinc.com/pic-labo/k_K04-B821-B5B51.jpg","https://image1.shopserve.jp/e-aocinc.com/pic-labo/llimg/k_K04-W621-01011.jpg"コクヨオンラインストア Yahoo!店 - COODE(コーデ)(オフィス
コクヨオンラインストア Yahoo!店 - COODE(コーデ)(オフィス
楽天市場】コクヨ ミーティングチェア COODE コーデ K04-W720CC
コクヨ KOKUYO ミーティングチェア COODE コーデチェア スタンダード
コクヨ KOKUYO ミーティングチェア COODE コーデチェア スタンダード
【楽天市場】コクヨ ミーティングチェア COODE コーデ K04
トップ ロールスノコ 切板(茶 プラスチック パールブルー 注目の福袋
楽天市場】コクヨ ミーティングチェア COODE コーデ K04-W720CC
楽天市場】コクヨ ミーティングチェア COODE コーデ K04-W720CC
楽天市場】コクヨ ミーティングチェア COODE コーデ K04-W720CC
コクヨ KOKUYO ミーティングチェア COODE コーデチェア スタンダード
レビューで送料無料 アルミ 61S Amazon 切板 板厚 120mm 100mm×900mm
トップ ロールスノコ 切板(茶 プラスチック パールブルー 注目の福袋
新品登場 生興 小型金庫 小型金庫 電子式耐火金庫 50KG (50kg
ラクラク納品】コクヨ ミーティングチェア CORne コルネ K07-DZ72 木製
トップ ロールスノコ 切板(茶 プラスチック パールブルー 注目の福袋
トップ ロールスノコ 切板(茶 プラスチック パールブルー 注目の福袋
トップ ロールスノコ 切板(茶 プラスチック パールブルー 注目の福袋
トップ ロールスノコ 切板(茶 プラスチック パールブルー 注目の福袋
トップ ロールスノコ 切板(茶 プラスチック パールブルー 注目の福袋
トップ ロールスノコ 切板(茶 プラスチック パールブルー 注目の福袋
楽天市場】コクヨ ミーティングチェア COODE コーデ K04-W720CC
ラクラク納品】コクヨ ミーティングチェア CORne コルネ K07-DZ72 木製
レビューで送料無料 アルミ 61S Amazon 切板 板厚 120mm 100mm×900mm
コクヨオンラインストア Yahoo!店 - COODE(コーデ)(オフィス
楽天市場】コクヨ ミーティングチェア 会議イス CORne コルネ K07-DZ72
ラクラク納品】コクヨ ミーティングチェア CORne コルネ K07-DZ72 木製
コクヨオンラインストア Yahoo!店 - COODE(コーデ)(オフィス
Amazon | 【配送・組立・設置込】 コクヨ 会議イス CK-750シリーズCK
コクヨオンラインストア Yahoo!店 - COODE(コーデ)(オフィス
コクヨ(KOKUYO) オリタタミイス CF-1SN
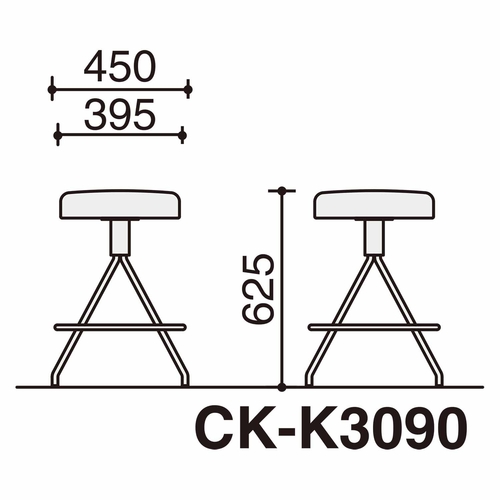
楽天市場】コクヨ スツール【CK-750】ミドルタイプ(塗装脚)【CK-750
【配送・設置込】 コクヨ 会議イス スタッキングチェア スプライン K11-M34-PW7E1 スチール脚 背ホワイトシェル/座ディープパープル
コクヨオンラインストア Yahoo!店 - COODE(コーデ)(オフィス
ラクラク納品】コクヨ ミーティングチェア CORne コルネ K07-DZ72 木製
回転式 ダイニングチェアー PUレザー ファブリック スチール脚 グレー
【配送・設置込】 コクヨ 会議イス スタッキングチェア スプライン K11-M34-PW7E1 スチール脚 背ホワイトシェル/座ディープパープル
【配送・設置込】 コクヨ 会議イス スタッキングチェア スプライン K11-M34-PW7E1 スチール脚 背ホワイトシェル/座ディープパープル
【配送・設置込】 コクヨ 会議イス スタッキングチェア スプライン K11-M34-PW7E1 スチール脚 背ホワイトシェル/座ディープパープル
コクヨ コーデ ミドルハイスツール 黒脚 黒|カウネット
コクヨオンラインストア Yahoo!店 - COODE(コーデ)(オフィス
コクヨオンラインストア Yahoo!店 - COODE(コーデ)(オフィス
楽天市場】コクヨ ミーティングチェア COODE コーデ K04-W720CC
コクヨ KOKUYO ミーティングチェア COODE コーデチェア スタンダード
コクヨ KOKUYO ミーティングチェア COODE コーデチェア スタンダード
【楽天市場】コクヨ ミーティングチェア COODE コーデ K04
トップ ロールスノコ 切板(茶 プラスチック パールブルー 注目の福袋
楽天市場】コクヨ ミーティングチェア COODE コーデ K04-W720CC
楽天市場】コクヨ ミーティングチェア COODE コーデ K04-W720CC
楽天市場】コクヨ ミーティングチェア COODE コーデ K04-W720CC
コクヨ KOKUYO ミーティングチェア COODE コーデチェア スタンダード
レビューで送料無料 アルミ 61S Amazon 切板 板厚 120mm 100mm×900mm
トップ ロールスノコ 切板(茶 プラスチック パールブルー 注目の福袋
新品登場 生興 小型金庫 小型金庫 電子式耐火金庫 50KG (50kg
ラクラク納品】コクヨ ミーティングチェア CORne コルネ K07-DZ72 木製
トップ ロールスノコ 切板(茶 プラスチック パールブルー 注目の福袋
トップ ロールスノコ 切板(茶 プラスチック パールブルー 注目の福袋
トップ ロールスノコ 切板(茶 プラスチック パールブルー 注目の福袋
トップ ロールスノコ 切板(茶 プラスチック パールブルー 注目の福袋
トップ ロールスノコ 切板(茶 プラスチック パールブルー 注目の福袋
トップ ロールスノコ 切板(茶 プラスチック パールブルー 注目の福袋
楽天市場】コクヨ ミーティングチェア COODE コーデ K04-W720CC
ラクラク納品】コクヨ ミーティングチェア CORne コルネ K07-DZ72 木製
レビューで送料無料 アルミ 61S Amazon 切板 板厚 120mm 100mm×900mm
コクヨオンラインストア Yahoo!店 - COODE(コーデ)(オフィス
楽天市場】コクヨ ミーティングチェア 会議イス CORne コルネ K07-DZ72
ラクラク納品】コクヨ ミーティングチェア CORne コルネ K07-DZ72 木製
コクヨオンラインストア Yahoo!店 - COODE(コーデ)(オフィス
Amazon | 【配送・組立・設置込】 コクヨ 会議イス CK-750シリーズCK
コクヨオンラインストア Yahoo!店 - COODE(コーデ)(オフィス
コクヨ(KOKUYO) オリタタミイス CF-1SN
楽天市場】コクヨ スツール【CK-750】ミドルタイプ(塗装脚)【CK-750
【配送・設置込】 コクヨ 会議イス スタッキングチェア スプライン K11-M34-PW7E1 スチール脚 背ホワイトシェル/座ディープパープル
コクヨオンラインストア Yahoo!店 - COODE(コーデ)(オフィス
ラクラク納品】コクヨ ミーティングチェア CORne コルネ K07-DZ72 木製
回転式 ダイニングチェアー PUレザー ファブリック スチール脚 グレー
【配送・設置込】 コクヨ 会議イス スタッキングチェア スプライン K11-M34-PW7E1 スチール脚 背ホワイトシェル/座ディープパープル
【配送・設置込】 コクヨ 会議イス スタッキングチェア スプライン K11-M34-PW7E1 スチール脚 背ホワイトシェル/座ディープパープル
【配送・設置込】 コクヨ 会議イス スタッキングチェア スプライン K11-M34-PW7E1 スチール脚 背ホワイトシェル/座ディープパープル
コクヨ コーデ ミドルハイスツール 黒脚 黒|カウネット
商品の情報
メルカリ安心への取り組み
お金は事務局に支払われ、評価後に振り込まれます
出品者
スピード発送
この出品者は平均24時間以内に発送しています